Learn about the Canadian Medical Protective Association and gain insights from lawyers who weigh in on the CMPA’s role in medical malpractice cases

Updated: 17 May 2024
Lawyers handling medical malpractice or negligence cases may be torn between prosecuting a claim against a medical professional or being destined to fail even before filing the case.
As for the latter part, most lawyers attribute it to the intervention of the Canadian Medical Protective Association or the CMPA in medico-legal cases in the country.
How strong is the influence of CMPA over the result of these cases? This article discusses this, along with the role of CMPA and the practical side of litigating malpractice and negligence cases from expert litigators.
What is the Canadian Medical Protective Association?
The Canadian Medical Protective Association (CMPA) is a non-profit organization that works as a mutual medical defence organization.
One of its functions is to defend members from medico-legal claims, or when a case is filed in court, including compensating victims and/or families of medical malpractice.
Although not required, almost all doctors and physicians in Canada are members of the CMPA.
How the CMPA works
CMPA’s roles in supporting its member-doctors, including their patients, are as follows:
Mutual medical defence
CMPA is not an insurance company. This means that insurance laws do not apply to them, and they do not underwrite its doctor-members' risks through insurance contracts.
This also means that when doctors apply to become a CMPA member, they subscribe to its principle of mutuality.
It allows members to be eligible for assistance when they’re faced with future medico-legal cases.
However, they’re also expected to practise in a manner consistent with the values of the medical profession.
Doctor-to-doctor support
Its member-doctors can also reach out to CMPA — either through phone or online — when seeking advice from peers. This includes:
- anything related to a patient’s medical care
- preventing harm to patients related to their healthcare
- situations where medico-legal difficulties may arise
Protection
CMPA members are given assistance when they’re faced with a medico-legal case, such as for malpractice or for negligence.
This includes providing legal representation to defend the members in civil suits. However, CMPA will first evaluate the case before defending members. It is only when the standard of care expected of medical professionals is met, according to the evaluation of their defence experts, that CMPA will step in. Otherwise, settlement with the victims and/or their families will be pursued as soon as possible.
The CMPA provides protection against the following types of medico-legal difficulties:
- civil and criminal cases for medical malpractice or negligence
- complaints lodged with a medical regulatory authority (e.g. provincial or territorial Colleges)
- coroner's inquest and other fatality inquiries
- billing audits and inquiries
- hospital complaints and privilege matters
- complaints for breach of privacy under a Canadian privacy law
- human rights complaints
Compensation to patients
The bulk of the resources of CMPA goes to the compensation of patients and/or their families, who are victims of malpractice and negligence of CMPA members.
This compensation can be a result of a settlement between the parties or a court decision against the erring defendant-CMPA member.
As a non-insurance company, CMPA is not restricted by pre-set compensation amounts or capped damages that are set by Canadian laws.
Other roles of CMPA
Aside from protecting members and compensating victims — which are the major roles of the CMPA — it also has other functions, such as:
- healthcare and public advocacy works
- publication of research through peer-reviewed journals
- collaborations on other healthcare stakeholders for a viable health care system
Eligibility for CMPA membership
To be a member of the CMPA, a person must:
- be a graduate of a degree in medicine
- be licensed or registered with a Canadian provincial or territorial medical regulatory authority
- pay the corresponding membership fee
Who funds the Canadian Medical Protective Association?
The CMPA is funded by membership fees collected from its member-doctors every year. These funds held by the CMPA are used in various ways, such as:
- for compensation: to compensate patients injured because of negligent medical care (or fault in Québec), such as settling cases and paying awards of damages
- for other legal costs: to support member-doctors who are accused of medical negligence
- for other purposes: advancing safe medical care, supporting the wellness of its physician-members, and other CMPA activities
As such, CMPA says that it does not receive any funding from any government or from Canadian taxpayers.
Reimbursement of CMPA dues
While doctors pay dues to be members of the CMPA, provinces pay the physicians back; in some provinces, up to 90%, less a small fee. This is due to the reimbursement agreements entered into by the provincial or territorial governments and medical associations or federations.
These agreements will also dictate the amount of reimbursement, which will then vary in every province or territory. CMPA says that it is not a party to these negotiations or agreements.
Know more about the CMPA’s financial structure and some of its key principles:
What is the role of the CMPA in medical malpractice cases?
Some lawyers contest the roles of the CMPA (as discussed above), which impacts the litigation of medical malpractice cases
However, some would also argue otherwise. As for both sides, suggestions on systematic reforms were also floated in the interest of justice for the victims and their families.
Overview of medical malpractice cases in Canada
The impact of the CMPA is already felt even before a medical malpractice case is accepted by a lawyer.
Paul Harte, a malpractice lawyer, says that in a typical year, he gets about 1,000 calls from potential clients who want his firm to take on their case for negligence or malpractice.
He might take on only about 25 of those cases. His decision is based on:
- his assessment of how much it would take to litigate the case
- whether it is winnable
- what the award could be
The reaction from those who have their cases turned down, he says, is something like “are you kidding me? The doctor made a mistake, and you’re telling me you can’t help me?”
It’s a difficult conversation to have, Harte admits, and certainly angers these clients against the entire medical service.
And the reason for this is at least partly because of the CMPA, he says.
This situation leaves zero incentive for the CMPA to reduce costs and be more efficient in protecting doctors, leading to a “scorched-earth” strategy.
The judge in Frazer v. Haukioja also used this same analogy, saying that CMPA-funded lawyers in this suit against an emergency doctor had pursued a “scorched-earth policy.”
In the ruling, it says that the defence put the plaintiffs to the test of proving all their claims on all issues of damages and liability, “and making the trial — at 20 days — needlessly long.”
The patient was successful, though, with an award of $1.9 million, and plaintiff fees and disbursement costs of almost $930,000.
Turning down medical malpractice cases
CMPA’s ability to vigorously defend doctors accused of malpractice means the threshold for taking on a case is high, says Harte.
“It is just not always economically viable to take on a doctor. It also creates a situation where the number of suits brought against doctors is lower than what it could be, and those cases that are litigated arguably produce better results for defendant doctors.”
While the threshold varies from lawyer to lawyer, he says somewhere around $250,000 is a typical settlement or award amount that makes a case worth taking on.
An example of one “economically unviable” case that he turned down involved a 22-year-old waiter with a benign tumor in his rib. After the operation, a problem occurred, allegedly because of a medical error, and the man had to have another operation.
However, “even though it’s a painful surgery, and the fellow had to take more time off, maybe the case is worth $20,000.”
Here is a case “where I think an error was clearly made,” he says. But he turned it down because the cost of litigating would far outweigh the award, given the CMPA’s defence-of-doctors mandate.
Data on medical malpractice cases in Canada
Harte says that because of how the CMPA works, there has been a steady reduction in legal actions.
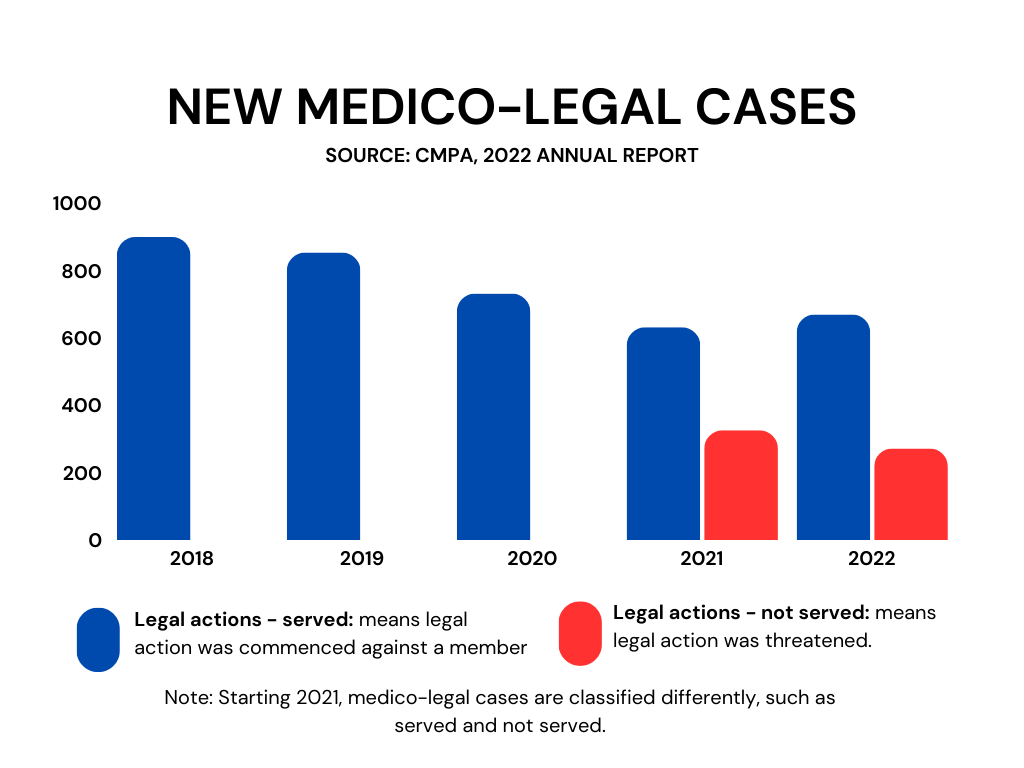
Photo caption: A graph showing CMPA new medico-legal cases from 2018-2022 broken down into legal actions – served and legal actions – not served
“It’s unlikely that there are fewer mistakes being made,” says Harte. “In fact, as we get more complicated medicine and more multi-disciplinary teams, the error rate is likely higher, not lower.”
“What’s happening is that, because of the impediments to suing, all kinds of meritorious claims are going without compensation,” he adds.
CMPA’s misunderstood mandate
The CMPA takes issue with arguments that lawyers use to criticize the Association.
Dr. Todd Watkins, Associate CEO with the CMPA, says the organization’s mandate is to “protect the professional integrity of physicians and promote safe medical care in Canada.”
Legal actions naturally call into question the integrity and reputation of the physician, he says.
Allegations that question the physician’s medical judgment and expertise “can be devastating to their future ability to practice, regardless of any monetary value.”
CMPA’s role in protecting doctors and physicians
When a patient initiates a claim against a physician-member, the role of the CMPA is to help the member in their defence if the care provided is medically defensible, says Watkins.
As for the “war chest” the CMPA has, Watkins says it is an unfair assessment that doesn’t reflect the Association’s approach to defending physicians. “The CMPA is committed to ensuring we can compensate patients and their families appropriately and in an amount that reflects their long-term care needs,” he says.
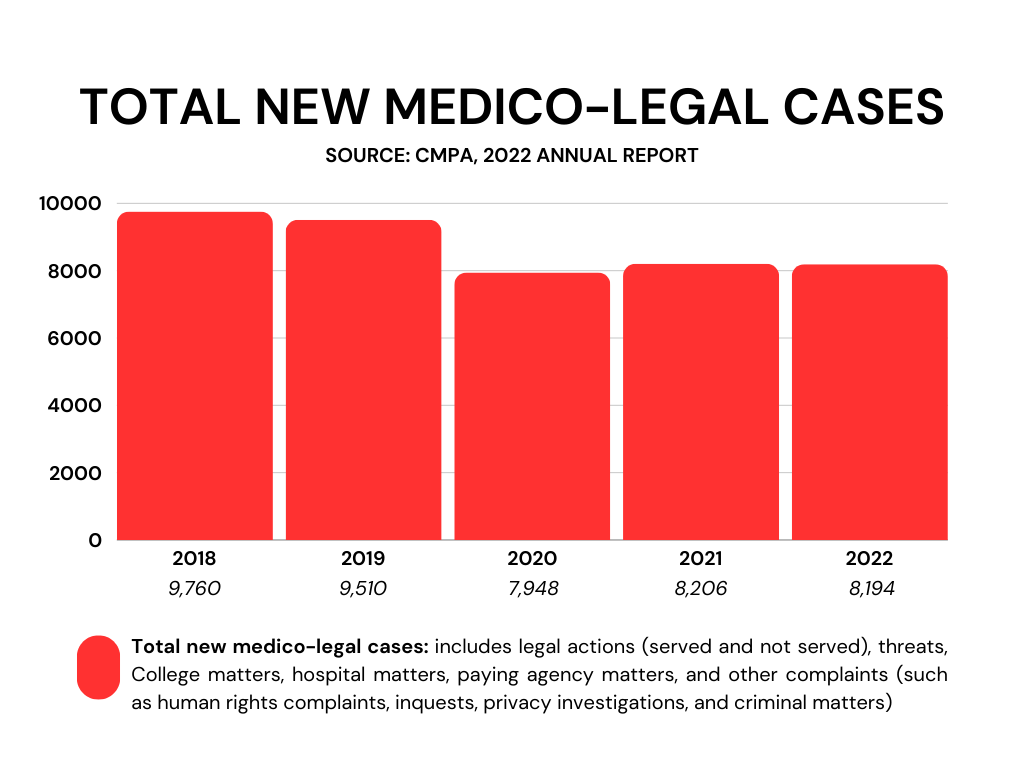
Photo caption: A graph showing total new medico-legal cases from 2018-2022 based on the Canadian Medical Protective Association’s 2022 annual report
Reasons other than the CMPA for weak malpractice cases
There are also plaintiff lawyers who don’t share Harte’s position. One of whom is Richard Halpern, a malpractice lawyer with Gluckstein Lawyers.
“The fact that most plaintiffs lose their case against doctors is not an indication of a problem with the system, it’s an indication the problem is with their case,” says Halpern.
“Judges don’t care how much money the CMPA has. If you go to trial against a doctor, and you lose the case, it’s [for] one of two reasons. Number one, your case didn’t have merit to begin with. Or number two, your lawyer didn’t handle the case properly.”
Not meeting the standards of torts law
Ryan Breedon, who spent several years working for a law firm that was counsel to the CMPA in Ontario, adds that medical malpractice is difficult to litigate and often expensive.
“It’s more about the law and the standard of proof that a plaintiff must meet. The approach of the CMPA is that if a case is considered defensible, they will defend it, and if not, it will be settled. I don’t take issue with that.”
Breedon adds that smaller cases often don’t get pursued because of how the system is set up. However, the flip side is that serious cases involving catastrophic injury are given settlements or awards to meet their care needs better.
Keeping the medical profession’s reputation
The question of reputation is important for members of the medical profession, says Breedon, as it can have lasting consequences.
He says that no procedure or treatment has a 100% chance of success, and someone will inevitably be on the wrong side of the statistics.
“These cases tend to be litigated in the communities where doctors live and work, and it’s not like a car accident with insurance, which will be settled.”
Not every bad outcome is medical malpractice
Halpern agrees, saying doctors are entitled to protect their reputation.
He adds that what a patient sees as malpractice in many cases is simply a bad outcome despite a proper standard of care.
Often, there is an underlying health issue with the patient, or the nature of the procedure comes with some known risks that the patient should have agreed to, through informed consent.
“Every procedure carries risk. Not all bad outcomes are due to bad care, but some are,” Halpern says. The role of the malpractice lawyer is to tease out which are which.
Harte says the system under the CMPA works on the “archaic view that doctors never make mistakes,” and too much time is spent defending that view.
The premise is, “if you admit to any kind of an error, that means that you’re inherently not a good doctor and your reputation takes a hit,” he says. That isn’t the case, he adds: “even excellent doctors make mistakes.”
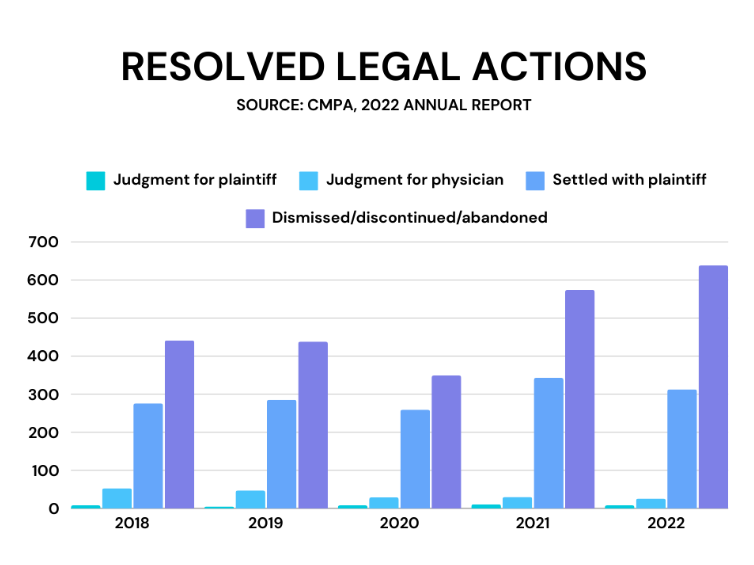
Photo caption: A graph showing resolved legal actions from 2018-2022 based on the Canadian Medical Protective Association’s 2022 annual report
Difficulty in looking for expert witnesses
The other challenge for malpractice plaintiffs is finding expert witnesses to testify whether a physician was negligent and if poor performance hurt the patient.
Harte says most cases rest on such evidence. Plaintiff lawyers say it’s challenging to find someone willing to testify against a colleague, and a culture of silence and “circling the wagons” exist.
However, Halpern says too much is made of this argument. He says it is true that many doctors are hesitant to criticize their colleagues, “but I’ve never had a case where I couldn’t find an expert who was prepared to give me an objective opinion.”
“It may be challenging for us to find experts who are prepared to testify. The fact is that there are always highly qualified, very competent experts who will look at your case and provide you with an objective opinion.”
Breedon agrees, saying the inability to find experts to testify for the plaintiff is “overblown.”
Funding of the CMPA and its legal implications
Arguments are also made when it comes to the government reimbursing most of the fees that doctors pay to be part of the CMPA.
Harte says this goes back to the rise of medical malpractice premiums in the 1980s, particularly in the US, and the fear that the same thing might happen here.
This resulted in medical associations arguing that this could mean losing doctors. So, they struck an agreement with the provinces outlining how the government would reimburse any increase in fees beyond a certain base level.
“Now, 30 years later, every specialty pays a different premium, but in general, 90% of the premium is reimbursed because that base rate has even been increased by inflation.”
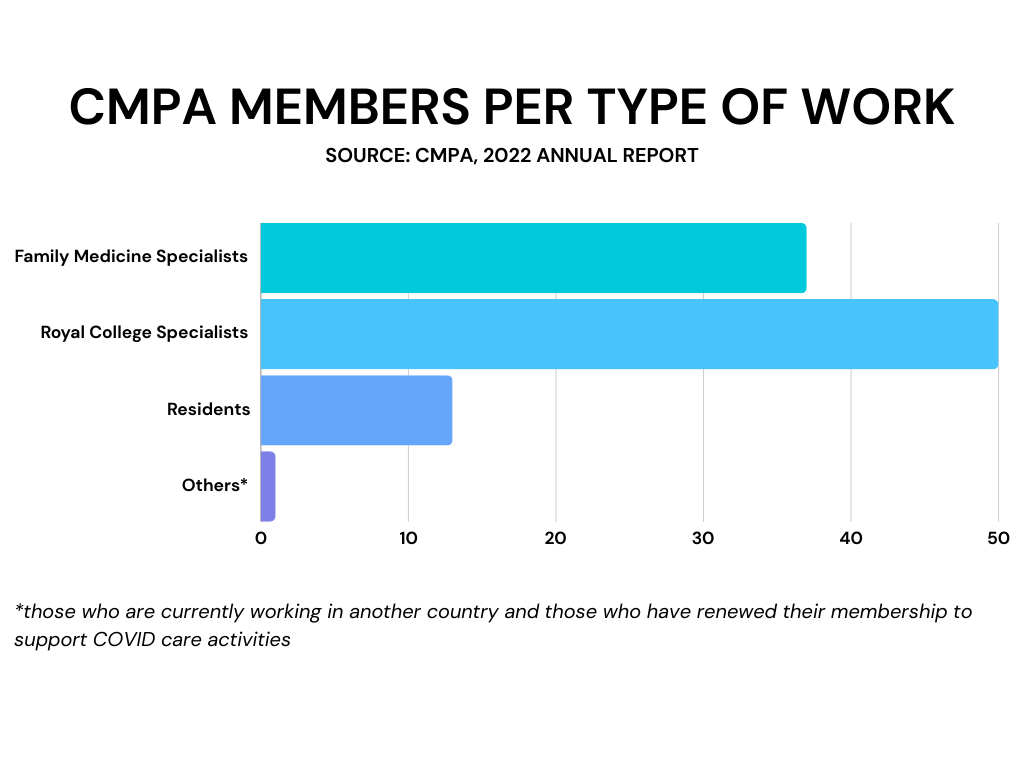
Photo caption: A graph showing a breakdown of the Canadian Medical Protective Association’s members per type of work in 2022
Benefits of how CMPA’s funding works
Halpern argues that subsidizing doctors on malpractice fees is a fair trade-off for Canada’s universal healthcare system.
“Because of that, the system has capped earnings for doctors. They are told what to charge for a procedure,” he says, arguing that doctors in Canada are probably underpaid relative to counterparts elsewhere.
“One of the things doctors were able to negotiate was partial subsidization of their premiums for malpractice. I think that’s completely appropriate.”
Addressing challenges when litigating medical malpractice cases
Solutions to some of the challenges of dealing with malpractice cases range from better education and training to no-fault insurance models used for vehicle accident claims.
This applies especially at the lower end of the potential award or settlement spectrum.
A shift on the CMPA’s mandate
Says Harte: “How do you fix the problem? The answer is changing the mandate of the CMPA from protecting doctors’ professional reputations to compensating victims of medical mistakes at the lowest reasonable cost.”
The current system leads to a huge dichotomy between winners and losers — with the most serious cases of proven malpractice well-compensated.
However, cases of lesser economic value are shut out of the system, he adds.
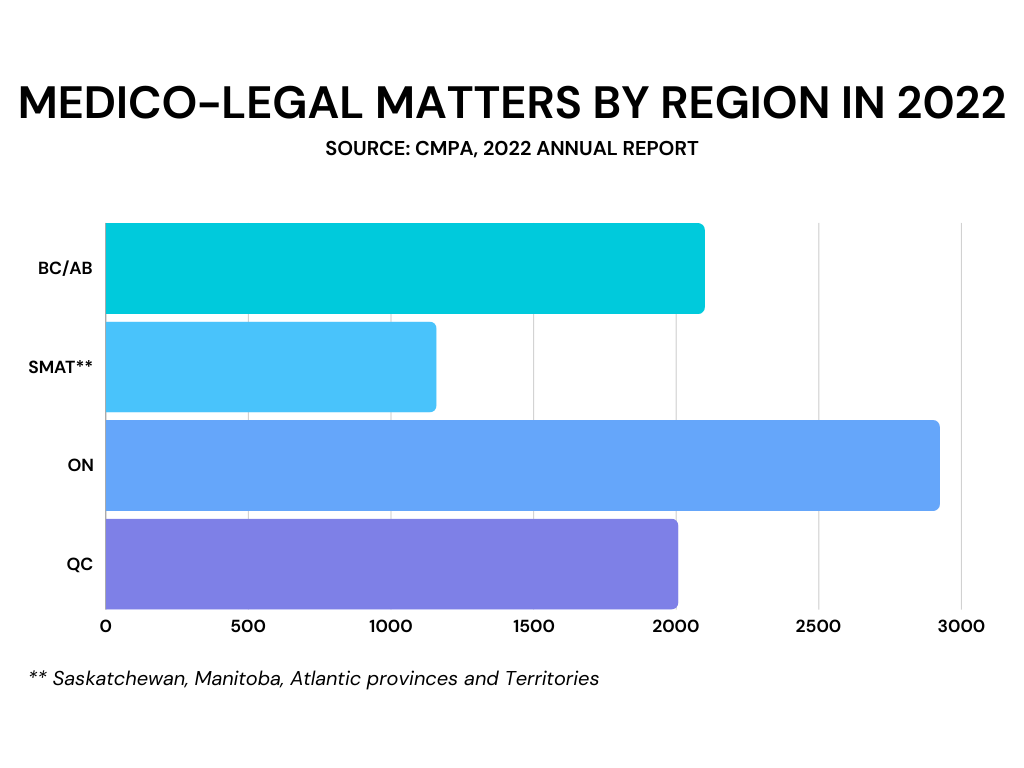
Photo caption: A graph showing breakdown of the Canadian Medical Protective Association’s medico-legal matters by region in 2022
Changing the system of litigation
A more inclusive system would lead to greater economic dealing of more cases, which would mean there would be more lawyers to represent malpractice litigants.
“We need to figure out a way to reduce transaction costs. And one of the ways you do that is by settling cases quickly by identifying any case that has to be resolved and settling it for a fair dollar,” Harte says.
Some caveats on these systemic changes
Breedon says the concept behind finding ways to make it more economical to deal with the cases below is good in theory. Still, he worries that such a system might mean less for the most catastrophic cases — where large settlements can impact quality of life.
Halpern says preserving the tort system for medical malpractice cases is crucial, explaining that versions of no-fault insurance in other countries have not worked well.
“The notion that there might be a correlation between no-fault medical compensation and improved patient safety is absurd.”
Indeed, eliminating the accountability and deterrent effect of the tort system means it is likely to put more patients at risk, he says.
As part of the Holland group, which includes CMPA lawyers and plaintiff lawyers, Halpern says any potential changes would not undermine the tort system.
“We encourage best practices, both on the defense side and on the plaintiff side. We encourage lawyers to carefully evaluate cases early to determine early on whether the standard of care or causation has been met...and then to proceed only with cases where you can establish that there is merit.”
Know more about the Canadian Medical Protective Association and medical malpractice cases by consulting with the Lexpert-ranked best medical negligence lawyers in Canada.










